Home / Categories / ZOCON-200MG
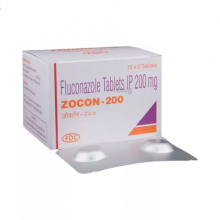
ZOCON-200MG
(2TX5S)
FLUCONAZOLE-200MG
ANTI-FUNGAL DRUGS
FDC LIMITED
Product Details
Fluconazole
Action
Indications
Contraindications
Route/Dosage
Interactions
Lab Test Interferences
Adverse Reactions
PrecautionsPatient Care Considerations
Administration/Storage
Assessment/Interventions
Patient/Family Education
(flew-KOE-nuh-zole)DiflucanClass: Anti-infective/Antifungal
 Action Interferes with the formation of fungal cell membrane, causing leakage of cellular contents and cell death.
Action Interferes with the formation of fungal cell membrane, causing leakage of cellular contents and cell death.
 Indications Oropharyngeal and esophageal candidiasis; vaginal candidiasis; prevention of candidiasis in bone marrow transplant; cryptococcal meningitis.
Indications Oropharyngeal and esophageal candidiasis; vaginal candidiasis; prevention of candidiasis in bone marrow transplant; cryptococcal meningitis.
 Contraindications Standard considerations.
Contraindications Standard considerations.
 Route/Dosage
Route/Dosage
Oropharyngeal or esophageal candidiasis
ADULTS: PO/IV 200 mg first day, followed by 100 mg qd thereafter for minimum of 2 wk for oropharyngeal candidiasis or 3 wk for esophageal candidiasis. CHILDREN: PO/IV 6 mg/kg on first day, followed by 3 mg/kg qd thereafter for minimum of 2 wk for oropharyngeal candidiasis or 3 wk (at least 2 weeks after symptom resolution) for esophageal candidiasis.
Vaginal candidiasis
ADULTS: PO 150 mg single dose.
Prevention of candidiasis in bone marrow transplant
ADULTS: PO/IV 400 mg once daily; in patients with anticipated severe granulocytopenia (< 500 neutrophils/mm3) start fluconazole several days before anticipated onset and continue 7 days after neutrophil count rises > 1000 cells/mm3.
Cryptococcal meningitis
ADULTS: PO/IV 400 mg first day, followed by 200 mg qd thereafter (400 mg may be used) for 10 to 12 wk after CSF culture is negative for initial meningitis; 200 mg qd for suppression of relapse of cryptococcal meningitis.
Candidemia and disseminated candida infections
CHILDREN: PO/IV 6 to 12 mg/kg/day.
Cryptococcal meningitis–12 mg/kg on first day, followed by 6 mg/kg/day (or 12 mg/kg/day based on medical judgment of patient's response). Recommended duration is 10 to 12 weeks after CSF becomes culture negative.
Suppression of relapse in AIDS patients– 6 mg/kg/day. NEONATES: Experience is limited to pharmacokinetic studies in premature newborns. Prolonged half-life has been noted. These children, in the first 2 wk of life, should receive the same mg/kg dosage as other children, but administered every 72 hr. After the first 2 wk, dose once daily.
 Interactions
Interactions
Anticoagulants (eg, warfarin): Anticoagulant effect may be increased. Alfentanil, benzodiazepines (eg, midazolam), buspirone, corticosteroids (eg, prednisone), nisoldipine, tacrolimus, vinca alkaloids (eg, vincristine): Levels may be elevated by fluconazole, increasing the risk of side effects and toxicity. Cyclosporine: Increased cyclosporine concentrations. Hydantoins (eg, phenytoin): Increased hydantoin levels. Rifamycins (eg, rifampin): Fluconazole plasma levels may be reduced, decreasing therapeutic effects.
 Lab Test Interferences Elevated transaminase levels. Coumadin: Increased PT may occur in patient receiving warfarin.
Lab Test Interferences Elevated transaminase levels. Coumadin: Increased PT may occur in patient receiving warfarin.
 Adverse Reactions
Adverse Reactions
CNS: Headache; seizures. DERM: Rash, exfoliative skin disorder. GI: Nausea; vomiting; abdominal pain; diarrhea. HEMA: Leukopenia; thrombocytopenia. HEPA: Hepatic reactions, including abnormal liver function test results, hepatitis, cholestasis, hepatic failure.
 Precautions
Precautions
Pregnancy: Category C. Lactation: Excreted in breast milk. Children: Efficacy not established; some patients 3 to 13 yr have been treated safely with 3 to 6 mg/kg/day. Anaphylaxis: Has occurred rarely. Dermatologic changes: Exfoliative skin disorders have been reported. Hepatic injury: Patients with abnormal liver function test results should be monitored for development of more severe hepatic injury. Immunocompromised patients: To prevent relapse, patients with AIDS and cryptococcal meningitis usually require maintenance therapy. Renal impairment: Dosage reduction based on creatinine clearance may be necessary.
PATIENT CARE CONSIDERATIONS
 Administration/Storage
Administration/Storage
- Do not administer if solution is cloudy or if precipitate is present.
- Do not add supplemental medications to IV infusion.
- Administer IV infusion at maximum rate of 200 mg/hr.
 Assessment/Interventions
Assessment/Interventions
- Obtain patient history, including drug history and any known allergies. Note renal impairment and sensitivity to fluconazole or other azoles.
- Obtain baseline BUN and creatinine levels.
- Ensure that baseline liver function tests have been obtained and monitor at regular intervals during treatment.
- Assess skin for rashes before beginning therapy and q 8 hr during treatment.
- If patient is receiving anticoagulants, assess for bleeding. Monitor coagulation studies closely.
- For patients also receiving coumadin, monitor PT for possible increased levels.
- If patient develops signs and symptoms of liver disease or new rash during therapy, notify physician.
 Patient/Family Education
Patient/Family Education
- Emphasize importance of taking drug for full course of therapy, which may be several weeks.
- Tell patient that if dose is missed, it should be taken as soon as possible. If close to next dose, do not double up; take next dose as scheduled.
- Instruct patient to report the following symptoms to physician: Nausea, vomiting, right upper quadrant abdominal pain, diarrhea, headache, rash.
Books@Ovid
Copyright © 2003 Facts and Comparisons
David S. Tatro
A to Z Drug Facts
