Home / Categories / TRYPTOMER-10MG
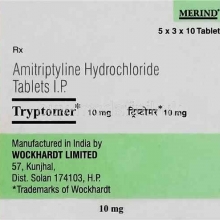
TRYPTOMER-10MG
(10)
AMITRIPTYLINE-10MG
TRICYCLIC ANTIDEPRESSANTS
MERIND
Product Details
Amitriptyline HCl
class: Tricyclic antidepressant
 Action Inhibits presynaptic reuptake of norepinephrine and serotonin in CNS.
Action Inhibits presynaptic reuptake of norepinephrine and serotonin in CNS.
 Indications Relief of depression. Endogenous depression is more likely to be allevated than are other depressive states. Unlabeled use(s): Management of chronic pain associated with migraine, tension headache, phantom limb pain, tic douloureux, diabetic neuropathy, peripheral neuropathy, cancer or arthritis; treatment of panic and eating disorders.
Indications Relief of depression. Endogenous depression is more likely to be allevated than are other depressive states. Unlabeled use(s): Management of chronic pain associated with migraine, tension headache, phantom limb pain, tic douloureux, diabetic neuropathy, peripheral neuropathy, cancer or arthritis; treatment of panic and eating disorders.
 Contraindications Hypersensitivity to any tricyclic antidepressant; use during acute recovery phase of MI; concomitant use with monoamine oxidase (MAO) inhibitors, except under close medical supervision; may block the antihypertensive action of guanethidine or similarly active compounds.
Contraindications Hypersensitivity to any tricyclic antidepressant; use during acute recovery phase of MI; concomitant use with monoamine oxidase (MAO) inhibitors, except under close medical supervision; may block the antihypertensive action of guanethidine or similarly active compounds.
 Route/Dosage
Route/Dosage
ADULTS: Titrate dosage over 2 wk to 1 mo. Give maintenance dose 6 mo to 1 yr. Do not interrupt therapy abruptly; reduce over 2 wk period. OUTPATIENTS: PO 75 to 150 mg/day in divided doses; give in evening or at bedtime because of sedative effects. HOSPITALIZED PATIENTS: PO 100 to 300 mg/day. ADOLESCENT & ELDERLY PATIENTS: PO 10 mg tid and 20 mg at bedtime. MAINTENANCE: PO 40 to 100 mg/day. PARENTERAL FORM: PO Do not use IV route. IM 20 to 30 mg qid. Change to oral dosing as soon as possible.
 Interactions
Interactions
Barbiturates, charcoal: May cause decreased blood levels of amitriptyline. Cimetidine, fluoxetine: May cause increased blood levels of amitriptyline. Clonidine: Use with product may result in hypertensive crisis. CNS depressants: Depressant effects may be additive. MAOIs: May cause hyperpyretic crises, severe convulsions, and death when given with amitriptyline.
 Lab Test Interferences None well documented.
Lab Test Interferences None well documented.
 Adverse Reactions
Adverse Reactions
CV: Orthostatic hypotension; hypertension; tachycardia; palpitations; arrhythmias; ECG changes. CNS: Confusion; hallucinations; disturbed concentration; decreased memory; delusions; nervousness; restlessness; agitation; panic; insomnia; nightmares; mania; exacerbation of psychosis; drowsiness; dizziness; weakness; emotional lability; numbness; tremors; extrapyramidal symptoms (eg, pseudoparkinsonism, movement disorders, akathisia); seizures. DERM: Rash; pruritus; photosensitivity reaction; dry skin; acne; itching. EENT: Conjunctivitis; blurred vision; increased IOP; mydriasis; tinnitus; nasal congestion; peculiar taste in mouth. GI: Nausea; vomiting; anorexia; GI distress; diarrhea; flatulence; dry mouth; constipation. GU: Impotence; sexual dysfunction; menstrual irregularities; dysmenorrhea; nocturia; urinary frequency; UTI; vaginitis; cystitis; urinary retention and hesitancy. HEMA: Bone marrow depression, including agranulocytosis; eosinophilia; purpura; thrombocytopenia; leukopenia. HEPA: Jaundice. META: Elevation or depression of blood sugar levels. RESP: Pharyngitis; rhinitis; sinusitis; cough. OTHER: Breast enlargement.
 Precautions
Precautions
Pregnancy: Category D. Lactation: Excreted in breast milk. Children: Not recommended for children < 12 yr. Changing from MAO inhibitor to amitriptyline: Waiting period of 7 to 10 days is necessary to prevent hypertensive crisis. Special risk patients: Caution is needed with history of seizures; urinary retention; urethral or ureteral spasm; angle-closure glaucoma or increased IOP; cardiovascular disorders; hyperthyroidism and patients receiving thyroid medication; hepatic or renal impairment; schizophrenia; paranoia. Serotonin syndrome: Some TCAs inhibit neuronal reuptake of serotonin and can increase synaptic serotonin levels.
PATIENT CARE CONSIDERATIONS
 Administration/Storage
Administration/Storage
- Use IM route only if patient is unable to take oral form.
- Give drug with or immediately after food or fluid and in late afternoon or at bedtime because of sedative effect. Tablets may be crushed.
- Store at room temperature and protect from light.
 Assessment/Interventions
Assessment/Interventions
- Obtain patient history, including drug history and any known allergies.
- Take vital signs and monitor during initial therapy.
- Assess patient's mental status, affect, energy level, sleeping, and eating habits and suicidal tendencies.
- Record I&O, noting bowel elimination pattern.
- Encourage high intake of fiber and fluid, and offer laxatives or stool softeners as necessary.
- Restrict amount of medication available to patient. Check patient's mouth after administration to detect possible hoarding of medication or noncompliance with therapy.
- Provide frequent oral hygiene.
- Assist patient in rising slowly. Supervise ambulation and institute measures to prevent falling.
- Monitor ECG, WBC with differential, serum glucose level, and cardiac, renal, and hepatic function regularly.
- Perform baseline and periodic leukocyte and differential counts and liver function studies.
- Document patient's mental status and vital signs every shift until response to therapy is evaluated.
- Monitor closely for oversedation, especially if patient is taking antihistamines, narcotic analgesics or sedatives/hypnotics.
- If systolic BP increases or decreases 10 to 20 mm Hg from baseline or if pulse rate or rhythm shows significant change, withhold drug and notify physician.
OVERDOSAGE: SIGNS & SYMPTOMS Confusion, agitation, hallucinations, seizures, status epilepticus, clonus, choreoathetosis, hyperactive reflexes, positive Babinski's sign, coma, cardiac arrhythmias, renal failure, flushing, dry mouth, dilated pupils, hyperpyrexia
 Patient/Family Education
Patient/Family Education
- Caution patient not to stop taking medication abruptly without consulting physician.
- Warn patient of the risk of seizure.
- Reinforce importance of follow-up visits to physician for monitoring drug's effectiveness and side effects.
- Explain that drug effects may not be evident for 4 to 6 wk but that side effects are usually noted early.
- Patient should complete the full course of therapy.
- Tell patient that side effects are reduced if drug is taken at bedtime.
- Advise patient that weight gain often results from increased appetite caused by drug.
- Inform patient that urine may turn blue-green.
- Emphasize the need for regular dental care because oral dryness can increase risk for dental caries.
- Instruct patient to report the following symptoms to physician: Blurred vision, sore throat, fever, increased heart rate, impaired coordination, difficult urination, excessive sedation, or seizures.
- Instruct patient to take sips of water frequently, suck on ice chips or sugarless hard candy, or chew sugarless gum if dry mouth occurs.
- Caution patient to avoid sudden position changes to prevent orthostatic hypotension.
- Instruct patient to avoid intake of alcohol beverages or other CNS depressants.
- Advise patient that drug may cause drowsiness, and to use caution while driving or performing other tasks requiring mental alertness.
- Caution patient to avoid exposure to sunlight, and to use sunscreen or wear protective clothing to avoid photosensitivity reaction.
- Instruct patient not to take otc medications without consulting physician.
Substitutes


