Home / Categories / RHOGAM INJ.300MCG/1500IU
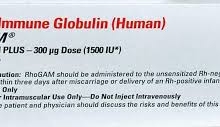
RHOGAM INJ.300MCG/1500IU
(1)
RHO(D) IMMUNE GLOBULIN HUMAN-300MCG
IMMUNOGLOBULIN
JOHNSON & JOHNSON LIMITED-PHARMA
Product Details
RHO(D) IMMUNE GLOBULIN HUMAN
Human Rho(D) immune globulin is a medicine given by intramuscular or intravenous injection that is used to prevent the immunological condition known as Rh disease (or hemolytic disease of newborn). Rho (D) immune globulin is available as a sterile, lyophilized or liquid gamma globulin (IgG) fraction containing antibodies to the Rh0 (D) antigen (D antigen) under the name Rhophylac (IM/IV). Immune globullin was purified via ion-exchange chromatography method and prepared from pools of human plasma, where the donors are Rho (D)-negative donors who have been immunized with Rho(D)-positive RBCs. It was approved by FDA as treatment for suppression of rhesus (Rh) isoimmunization or chronic immune thrombocytopenic purpura (ITP) in adults.
Indication
Indicated for suppression of rhesus (Rh) isoimmunization in nonsensitized Rho (D)-negative women with an Rh-incompatible pregnancy, or in Rho (D)-negative individuals transfused with Rh0(D)-positive red blood cells (RBCs) or blood components containing Rh0(D)-positive RBCs. Also indicated in Rh0(D)-positive, non-splenectomized adult patients with chronic immune thrombocytopenic purpura (ITP) to raise platelet counts.
Associated Conditions
Associated Therapies
Pharmacodynamics
15000 international unit (IU) contains sufficient anti-Rho (D) to effectively suppress the immunizing potential of approximately 17mL of Rho (D) (D-positive) red blood cells [12]. Human Rho(D) immune globulin therapy prevents immunization to Rho (D)-positive red blood cells (RBC) by inducing antibody-mediated immunosuppression (AMIS) effectively clearing Rho-positive RBCs by rapidly binding to them. This prevents Rho-negative mothers to produce alloantibodies to paternally inherited RhD antigen expressed on fetal erythrocytes and cause haemolytic diseases of the newborn. Rho immune globulin increase platelet counts and reduce bleeding in Rho-positive patients with ITP by inhibiting autoantibody-mediated platelet clearance.
Mechanism of action
The mechanism of action of Rho(D) immune globulin therapy is unclear. It is suggested that Rho immune globulin predominantly prevents the antibody response during incompatible pregnancy by accelerating the phagocytosis of RBC's and clearance from the circulation before the recognition by the immune system. IgG-opsonized RBCs may interact with activating IgG receptors (FcγRs) on effector cells and elicit phagocytosis via mononuclear phagocytic system, primarily by macrophages. IgG may also stimulate complement activation on the RBC surface, followed by RBC lysis or complement receptor-mediated phagocytosis but to smaller extent [4]. Rho-specific IgG may inhibit the late stages of B cell activation by being internalized with Rho antigen by B cells, which alters the antigen processing and presentation. In response to the IgG-antigen complex formation, the immune globulin enhances the presentation of specific peptides and proliferation of epitope-specific T cells [4]. Therapeutic efficacy of Rho (D) immune globulin in chronic immune thrombocytopenic purpura (ITP) may be explained by FcR blockade as well as the increase in the platelet count by substituting antibody-coated RBCs for antibodycoated platelets [2]. In vitro studies of cytokine expression in human monocytes and granulocytes exposed to anti-D coated red blood cells have demonstrated enhanced secretion of interleukin 1 receptor antagonist resulting in down-regulation of FcγR mediated phagocytosis. Murine models show that RBC-specific antibodies can increase platelet counts by down-regulating FcγRIIIa on splenic macrophage, which is an opposing effect as predicted in intravenous Rho IgG.
Absorption
In patients undergoing therapy for Rh isoimmunization suppression, Rho(D) immune globulin titers were detected in all women up to at least 9 weeks following either intravenous or intramuscular administration. Following intravenous administration of a single 1500 IU (300 mcg) dose, peak serum levels of Rh0(D) immune globulin ranged from 62 to 84 ng/mL after first day. The levels ranged from 7 to 46 ng/mL and were achieved between 2 and 7 days following intramuscular injection. The absolute bioavailability achieved following IM administration is 69%.
Volume of distribution
A single dose of 300ug Rho(D) Immune Globulin through intramuscular injection displays a Vd of 8.59L [13].
Protein binding
Not Available
Metabolism
Rho (D) immune globulin is expected to undergo nonspecific catabolism.
Route of elimination
Human immune globulin and the fragments can be detected in feces and urine.
Half life
The half life is 16 ± 4 days following IV administration and 18 ± 5 days following IM administration.
Clearance
Mean systemic clearance following IV administration is 0.20 ±0.03 mL/min. Mean apparent clearance following IM administration is 0.29 ± 0.12 mL/min.
Toxicity
Most serious adverse reactions in patients with ITP include intravascular hemolysis, anemia, acute renal insufficiency, and death. In patients treated for Rh isoimmunization suppression, common adverse effects include nausea, dizziness, headache, pain at injection site and malaise. Common adverse effects in patients with ITP include chills, pyrexia, mild extravascular hemolysis and headache.
SOURCE:DRUGBANK
Substitutes
Substitutes not found for RHOGAM INJ.300MCG/1500IU