Home / Categories / CIZODOL-P-1.5MG
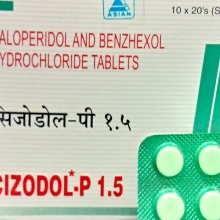
CIZODOL-P-1.5MG
(10TX20S)
HALOPERIDOL-5MG
BENZHEXOL-2MG
ANTI-PSYCHOTICS
ASIAN PHARMACEUTICALS-SOLAR-DIVISION
Product Details
Haloperidol
A to Z Drug Facts
| Haloperidol |
| (HAL-oh-pehr-i-dahl) |
Haldol,  Apo-Haloperidol, Novo-Peridol, Peridol, PMS-Haloperidol, PMS-Haloperidol LA, Apo-Haloperidol, Novo-Peridol, Peridol, PMS-Haloperidol, PMS-Haloperidol LA Apo-Haloperidol, Novo-Peridol, Peridol, PMS-Haloperidol, PMS-Haloperidol LA, Apo-Haloperidol, Novo-Peridol, Peridol, PMS-Haloperidol, PMS-Haloperidol LA |
| Haloperidol Decanoate |
Haldol Decanoate 50, Haldol Decanoate 100,  Haldol LA, Rho-Haloperidol Decanoate, Haldol Decanoate 100, Haldol LA, Rho-Haloperidol Decanoate, Haldol Decanoate 100,  Haldol LA, Rho-Haloperidol Decanoate Haldol LA, Rho-Haloperidol Decanoate |
| Class: Antipsychotic/Butyrophenone |
 Action Has antipsychotic effect, apparently due to dopamine-receptor blockage in CNS.
Action Has antipsychotic effect, apparently due to dopamine-receptor blockage in CNS.
 Indications Management of psychotic disorders; control of Tourette's disorder in children and adults; management of severe behavioral problems in children; short-term treatment of hyperactive children. Long-term antipsychotic therapy (haloperidol decanoate). Unlabeled use (s): Treatment of phencyclidine (PCP) psychosis; antiemetic.
Indications Management of psychotic disorders; control of Tourette's disorder in children and adults; management of severe behavioral problems in children; short-term treatment of hyperactive children. Long-term antipsychotic therapy (haloperidol decanoate). Unlabeled use (s): Treatment of phencyclidine (PCP) psychosis; antiemetic.
 Contraindications Severe toxic CNS depression or comatose states from any cause; Parkinson's disease.
Contraindications Severe toxic CNS depression or comatose states from any cause; Parkinson's disease.
Individualize dosage. ADULTS: PO 0.5 to 40 mg/day in divided doses; up to 100 mg/day in severe cases. ADULTS: IM 0.5 to 5 mg q 60 min; however, q 4 to 8 hr may be satisfactory.
HALOPERIDOL DECANOATE
ADULTS: IM (deep injection) Initial dose is 10 to 20 times oral dose. Usually given q 4 wk. CHILDREN 3 to 12 YR: PO Initially 0.5 mg/day. Increase in 0.5 mg increments every 5 to 7 days until therapeutic effect is achieved. Total dose divided and given bid or tid.
Anesthetics, opiates, alcohol: May increase CNS depressant effects. Anticholinergics: May increase anticholinergic effects. May worsen schizophrenic symptoms, decrease haloperidol serum concentrations, and lead to tardive dyskinesia. Carbamazepine: May decrease effects of haloperidol. Lithium: May induce disorientation, unconsciousness, and extrapyramidal symptoms.
 Lab Test Interferences Pregnancy tests: False-positive results may occur; less likely to occur with serum test. Protein-bound iodine: Increases have been reported.
Lab Test Interferences Pregnancy tests: False-positive results may occur; less likely to occur with serum test. Protein-bound iodine: Increases have been reported.
CV: Orthostatic hypotension; hypertension; tachycardia; ECG changes. CNS: Tardive dyskinesia; tardive dystonia; insomnia; restlessness; anxiety; euphoria; agitation; drowsiness; depression; lethargy; headache; confusion; vertigo; seizures; exacerbation of psychotic symptoms; pseudoparkinsonism (eg, mask-like face, drooling, pill rolling, shuffling gait, inertia, tremors, cogwheel rigidity); muscle spasms; dyskinesia; akathisia; oculogyric crises; opisthotonos; hyperreflexia. DERM: Maculopapular and acneiform skin reactions; photosensitivity; hair loss. EENT: Cataracts; retinopathy; visual disturbances; mydriasis; increased IOP; nasal congestion. GI: Dyspepsia; anorexia; diarrhea; hypersalivation; nausea; vomiting; dry mouth. GU: Impotence; sexual dysfunction; priapism; urinary hesitancy or retention. HEMA: Agranulocytosis; leukopenia; leukocytosis; anemia. HEPA: Jaundice; impaired liver function. RESP: Laryngospasm; bronchospasm; increased depth of respiration. OTHER: Menstrual irregularities; breast enlargement; lactation; gynecomastia; hyperglycemia; hypoglycemia; hyponatremia; elevated prolactin levels; adynamic ileus (may lead to death).
Pregnancy: Haloperidol: Safety not established. Haloperidol decanoate: Category C. Lactation: Excreted in breast milk. Children: Do not use in children < 3 yr. IM form not recommended in children. Elderly or debilitated patients: More susceptible to effects; consider lower dose. Special risk patients: Use drug with caution in patients with cardiovascular disease or mitral insufficiency, history of glaucoma, EEG abnormalities or seizure disorders, prior brain damage, or hepatic or renal impairment. Antiemetic effects: Due to suppression of cough reflex, aspiration of vomitus possible. CNS effects: May impair mental or physical abilities, especially during first few days of therapy. Hepatic effects: Jaundice usually occurs in 2 to 4 wks of treatment and is considered a hypersensitivity reaction. Usually reversible. Neuroleptic malignant syndrome (NMS): Has occurred and is potentially fatal. Signs and symptoms are hyperpyrexia, muscle rigidity, altered mental status, irregular pulse, irregular BP, tachycardia, and diaphoresis. Sensitivity to neuroleptic drugs: May require lower dosage. Sudden death: Has been reported; predisposing factors may be seizures or previous brain damage. Flareup of psychotic behavior may precede death. Tardive dyskinesia: Syndrome of potentially irreversible, involuntary dyskinetic movements may develop. Prevalence is highest in elderly, especially women. Use smallest effective dose for shortest period of time needed. Tartrazine sensitivity: Note that tartrazine is a component of this product.
| PATIENT CARE CONSIDERATIONS |
|
- Dilute liquid in fruit juice.
- Observe patient carefully when administering to ensure medication is taken and not hoarded.
- Give with food or full glass of water to minimize GI irritation.
- Replace injectable form by oral form as soon as possible.
- Protect liquid concentrate from light and store in opaque bottle.
- Obtain patient history, including drug history and any known allergies.
- Observe patient for extrapyramidal symptoms and tardive dyskinesia. Notify health care provider if symptoms develop.
- Assess patient's mental status throughout therapy.
- Evaluate CBC and liver function studies before and periodically throughout therapy.
- Assess I & O and bowel function frequently.
- Observe safety precautions such as close patient supervision and removal of harmful objects from patient's environment.
- Increase bulk and fluids in patient's diet to minimize constipation.
- Keep the patient recumbent after IM injection to reduce hypotension.
|
||||
- Caution patient to avoid exposure to sunlight and to use sunscreen or wear protective clothing to avoid photosensitivity reaction.
- Instruct patient to avoid intake of alcoholic beverages or other CNS depressants.
- Instruct patient to use mouth rinses, good oral hygiene, and sugarless gum or candy to relieve dry mouth.
- Advise patient to avoid sudden position changes to prevent orthostatic hypotension.
- Instruct patient to report these symptoms to health care provider: Drooling, tremors, shuffling gait, restlessness, muscle spasms, aching or numbness, weakness, impaired vision, sore throat, fever, bleeding or bruising, rash, or jaundice.
- Inform patient of possible hair loss.
- Advise patient that drug may cause drowsiness and to use caution while driving or performing other tasks requiring mental alertness.
Books@Ovid
Copyright © 2003 Facts and Comparisons
David S. Tatro
A to Z Drug Facts
BENZHEXOL
One of the centrally acting muscarinic antagonists used for treatment of parkinsonian disorders and drug-induced extrapyramidal movement disorders and as an antispasmodic
Indication
Indicated for the treatment of parkinson's disease and extrapyramidal reactions caused by drugs.
Associated Conditions
- Extrapyramidal symptoms caused by butyrophenones
- Extrapyramidal symptoms caused by dibenzoxazepines
- Extrapyramidal symptoms caused by phenothiazines
- Extrapyramidal symptoms caused by thioxanthenes
- Parkinsonism post encephalitic
- Arteriosclerotic Parkinsonism
- Extrapyramidal disorders
- Idiopathic Parkinsonism
Pharmacodynamics
Trihexyphenidyl is an anticholinergic used in the symptomatic treatment of all etiologic groups of parkinsonism and drug induced extrapyramidal reactions (except tardive dyskinesia). Trihexyphenidyl possesses both anticholinergic and antihistaminic effects, although only the former has been established as therapeutically significant in the management of parkinsonism.
Mechanism of action
Trihexyphenidyl is a selective M1 muscarinic acetylcholine receptor antagonist. It is able to discriminate between the M1 (cortical or neuronal) and the peripheral muscarinic subtypes (cardiac and glandular). Trihexyphenidyl partially blocks cholinergic activity in the CNS, which is responsible for the symptoms of Parkinson's disease. It is also thought to increase the availability of dopamine, a brain chemical that is critical in the initiation and smooth control of voluntary muscle movement.
Toxicity
Symptoms of overdose include mydriasis, dryness of mucous membranes, red face, atonic states of bowels and bladder, and hyperthermia in high doses. Central consequences are agitation, confusion, and hallucinations. An untreated overdose may be fatal, particular in children. Premortal signs are respiratory depression and cardiac arrest.
SOURCE:DRUGBANK
.
Substitutes
Substitutes not found for CIZODOL-P-1.5MG
 Route/Dosage
Route/Dosage Interactions
Interactions Adverse Reactions
Adverse Reactions Precautions
Precautions Administration/Storage
Administration/Storage Assessment/Interventions
Assessment/Interventions Patient/Family Education
Patient/Family Education